Primary lung carcinoma spreading to pulmonary vessels and presenting as a thromboembolic disease is quite rare and only few individual cases have been reported in the English literature.1-3 The prognostic significance of pulmonary vessel invasion by lung carcinoma is unclear and the treatment is challenging. We aim to describe an unusual case of sarcomatoid carcinoma of the lung characterised by its hilar localization.1,2
Case report
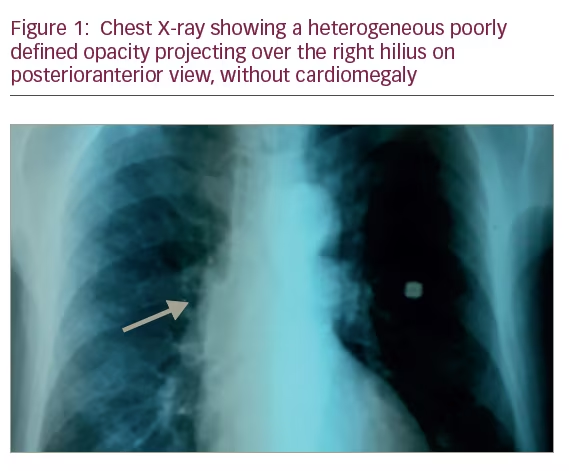
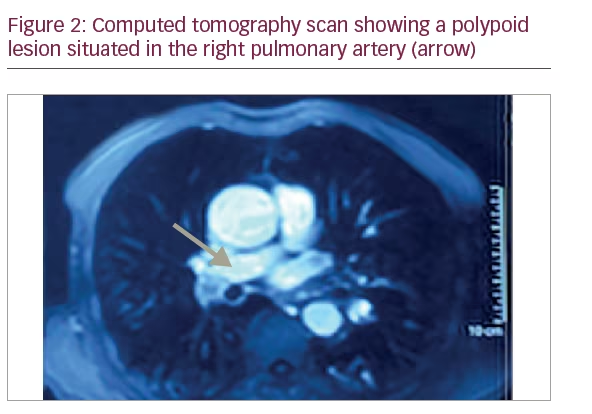
A 68-year-old man, 80 pack-year smoker, consulted for a 4-month-lasting effort dyspnea of New York Heart Association (NYHA) functional class II and dry cough. Physical examination revealed a grade III/IV ejection systolic murmur in the aortic area. Chest X-ray showed a heterogeneous poorly defined opacity of the right hilius without cardiomegaly (Figure 1). Electrocardiogram showed a regular sinusoidal rhythm and a tachycardia at 100 beats/min without signs of left ventricular hypertrophy. A two-dimensional (2D) transthoracic echocardiography (TTE) showed a severe aortic stenosis. The left ventricular ejection fraction was estimated to 70%. There was no pulmonary arterial hypertension. The pulmonary artery systolic pressure was estimated to 30 mm Hg. A computed tomography (CT) scan revealed a thrombus in the lower branch of the right pulmonary artery of tumoural appearance extending to the right lower lobe artery (Figure 2). Bronchial fibroscopy was normal. No distant metastasis was revealed by the cerebral CT scan or the abdominal CT scan. The lung function was within normal values. Surgical resection of the arterial process and aortic replacement was decided.
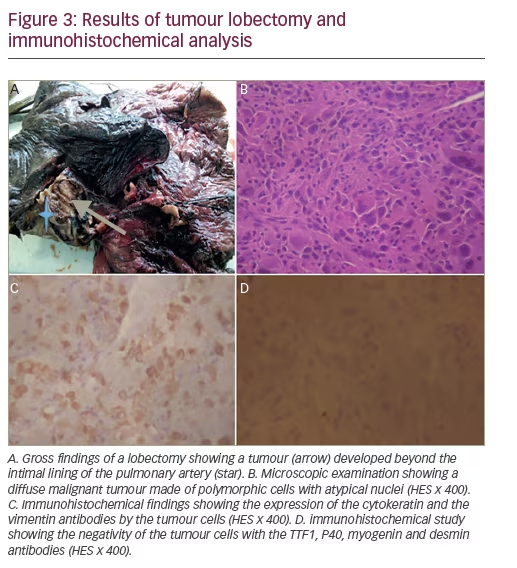
Surgical resection was performed through a median vertical sternotomy. The procedure consisted of a right intra pericardial pneumonectomy with aortic valve replacement by a mechanical valve. A mediastinal lymph node dissection was also performed. Postoperative macroscopic examination of the resected specimen showed a 2 cm tumour encompassing the pulmonary artery and developing into the sub-intima without endoluminal component (Figure 3A). The extemporaneous exam concluded to a sarcomatous tumour. Definitive microscopic findings consisted in a malignant proliferation with wide necrosis composed of tumour cells of variable size with abundant eosinophilic cytoplasm and atypical nuclei. Some tumour cells were multinucleated (Figure 3B). Immunohistochemical study revealed the co-expression of cytokeratin and vimentin antibodies by the tumour cells (Figure 3C and D). Other antibodies including anti-smooth muscle actin and desmin weren’t expressed, ruling out the diagnosis of a muscle differentiated tumour. The mediastinal lymph nodes dissected were benign.
These morphological and immunohistochemical features were consistent with a primary sarcomatoid carcinoma of the lung invading the pulmonary artery classified as a pT1N0M0 tumour. Molecular studies highlighted no epidermal growth factor receptor (EGFR), Her mutations, anaplastic lymphoma kinase (ALK) translocation or c-met amplification.
There were no postoperative serious complications except for an atelectasis with oxygen dependency. This complication was managed by a non-invasive ventilation and chest physiotherapy with a good outcome. The patient was discharged 18 days after the surgical resection. He is still
followed by the oncologist, and after 4 months of follow-up, presented no complications.
Discussion
This case was interesting because it illustrated a rare presentation of sarcomatoid carcinoma of the lung. This tumour is very rare and mainly peripherally localised. The hilar localisation induced nonspecific presenting symptoms, which were confused with pulmonary thromboembolism.3 The artery obstruction may be caused by an intrinsic or extrinsic tumour.4 In the case reported here, the tumour development was sub-intimal without an intra luminal development. It was revealed by the CT, which represents the standard reference method for the diagnosis of acute pulmonary thromboembolism and was also reported by some authors to have prognostic value.5Sarcomatoid carcinoma of the lung accounts for 0.3 to 0.1% of all lung malignancies. It was recognised as a distinct entity by the World Health Organization classification (WHO 1999), updated in 2004 and 2015.1 It is defined as a poorly differentiated non-small cell carcinoma that contains sarcomatous component or sarcoma-like elements. It represents an overall continuum of epithelial and mesenchymal differentiation.1,6 The diagnosis is based on the microscopic and the immunohistochemical examination. Immunohistochemical analysis shows cytokeratin positivity (most often AE1AE3, CAM5.2, CK18, CK7). Vimentin, carcinoembryonic antigen (CEA) and smooth muscle markers can also be positive, but positivity of epithelial markers is not essential if components of conventional cancer are morphologically present.6
Surgical resection is the mainstay treatment. Adjuvant therapy is sometimes used but is poorly effective.1,6 The prognosis is worse than the prognosis of other non-small cell lung carcinomas.1 It essentially depends on the size and extent of the tumour. Some studies suggest that blood vessel invasion is a major prognostic factor associated with shorter survival.3,7,8 In this case, the tumour had invaded the pulmonary artery. The rarity of this tumour growth pattern makes it difficult to diagnose. The blood invasion observed in sarcomatoid carcinoma is thought to lead to dissemination of the tumour in the pulmonary
circulation, resulting in multiple intrapulmonary metastases.8 However, in our case, such pathological findings were not observed.Thus, even when macroscopic tumour invasion to the pulmonary artery is observed, complete surgical resection of the tumour may offer a better prognosis.9
Conclusion
We have presented a case of lung sarcomatoid carcinoma invading the pulmonary artery. This mode of tumour extension is rare and its prognostic significance remains unclear, especially in such a subtype. We aimed to highlight that pulmonary artery invasion by a lung carcinoma is part of the differential diagnosis of chronic thromboembolic disease. Although blood vessel invasion is generally an ominous prognostic factor, curative surgical resection should improve the prognosis







