Despite huge strides in the fight against TB, the WHO’s Global Tuberculosis Report 2019 ranked Bangladesh sixth among the countries with the highest number of TB cases (4% of the global total), and seventh among the top 10 countries with the widest gap between notified and incident TB cases.1 Funding for TB programmes remains challenging and an obstacle for the national TB control programme.2 The challenges of performing diagnostic testing, due to the lack of consistent availability of tests, further adds to fragmented TB control measures. In Bangladesh, the GeneXpert® (Cepheid, Sunnyvale, CA, USA) test is performed, and is required in patients where TB is highly suspected but who have negative sputum smears or treatment failure.3 Confirmation and diagnosis of TB by the gold standard test of culture is not widely available.3 This leads to non-recognition of other mycobacteria as a primary diagnosis, comorbidity or co-infection.
What are non-tuberculous mycobacteria?
Non-tuberculous mycobacteria (NTM), also known as atypical mycobacteria, are a group of mycobacteria abundant in soil and water. NTM organisms include all mycobacteria except Mycobacterium tuberculosis, M. leprae and M. ulcerans.4 These ubiquitous environmental mycobacteria have a thick, lipid-rich, hydrophobic cell wall and the ability to form a biofilm, enabling them to survive at high temperatures and acidic pH, and resist heavy metals, disinfectants, chlorination and antibiotics. They may be present in food, drinking water, drainage water, household plumbing, soils, brackish marshes, water bodies like rivers and estuaries, dust, and in the skin, droppings or saliva of animals and fish. Additionally, they have been recovered from overhead showers and hospital water systems.5
NTM are opportunistic, low-grade pathogens capable of colonizing or infecting the lungs, skin, lymph nodes and soft tissues, besides presenting as disseminated infection in immunocompromised individuals, or co-existing with or following TB. The most common site of infection is the lungs, leading to pulmonary NTM, which closely mimicks TB, clinically. The most common organisms associated with this disease are M. avium complex (MAC), M. kansasii, M. xenopi and M. abscessus.6 These are prevalent in individuals with underlying conditions such as chronic obstructive pulmonary disease (COPD), cystic fibrosis and non-cystic fibrosis bronchiectasis, and in lung transplant recipients and patients with human immunodeficiency virus (HIV). It is postulated that transmission occurs via inhalation, ingestion or implantation.7 However, genomic studies have indicated the possibility of human-to-human transmission in some cases.8 In addition, a strong association exists with alcoholism and oesophageal disorder such as achalasia.9
A study, conducted from 2007 to 2009, found that respiratory samples from 17 patients yielded the same NTM species as those recovered from their household water and biofilm samples. Among these, isolates from seven patients had the same repetitive sequence-based polymerase chain reaction (PCR) DNA fingerprint as at least one NTM isolate recovered from household plumbing.10 A recent study, published in 2019, established household water systems as the source of infection by comparing the genotypes of the NTM species recovered from respiratory samples and household plumbing biofilms, using methods such as variable-number tandem-repeat genotyping and whole-genome sequencing. The authors concluded that the municipal water was the source of the infection, since all patients lived in the same community and were serviced by the same water plant.11
NTM have been recognized as an emerging public health problem in many countries. Unlike TB – and with a few exceptions in some states of the USA and in Queensland, Australia – NTM is not a reportable disease in most countries. The most common NTM species isolated worldwide are MAC, M. gordonae and M. xenopi.12 In 2013, Hoefsloot et al. observed that MAC was prevalent in almost all countries.6 While a 2004 study showed that the number of isolates with MAC and M. xenopi have seen an upward trend, the numbers for M. gordonae and M. kansasii have experienced a fall.12
Japan reported only three NTM-related deaths in 1970, which climbed to 1,121 in 2010. The crude NTM-related mortality rate increased from 0.003/100,000 in 1970 to 0.870/100,000 in 2010.13 Meanwhile, 2,990 NTM-related deaths were recorded from 1999 to 2010 in the USA. The mean age-adjusted mortality rate was 0.1 per 100,000 person-years. Hawaii had the highest mortality rate at 0.29 per 100,000 person-years, while Louisiana had the second highest rate of 0.17 per 100,000 person-years.14
Disease pathology
Since pulmonary NTM is caused mainly by MAC throughout the world,4 we will focus on MAC lung disease in the form of a clinical overview:
- Fibro-cavitary pulmonary disease: most commonly present in smokers, males and/or those with underlying lung conditions, such as COPD, silicosis or pneumoconiosis, or prior TB infection. Infected patients are usually between 50 and 70 years of age. It usually involves the apical and posterior segments of the upper lobe.15
- Non-cystic fibrosis bronchiectasis disease, also known as ‘Lady Windermere syndrome’: occurs in women between 40 and 80 years of age, who have a low body mass index and no known pre-existing lung disease. Mainly described in Caucasian women, this disease is associated with scoliosis, pectus excavatum and mitral valve prolapse.16
- Hypersensitivity pneumonitis, also known as ‘hot-tub lung’: occurs in patients after being exposed to aerosolized MAC in hot-tubs, medicinal pools or metalworking fluid.15
- Disseminated disease: this may occur in immunocompromised patients, which include patients with HIV with CD4+ T-lymphocyte <50 cells/mm3, transplant recipients and those on tumour necrosis factor-alpha antagonists. In disseminated disease, respiratory colonization without any symptoms is not uncommon.
Diagnostic criteria of non-tuberculous mycobacterial pulmonary disease
The diagnosis of pulmonary NTM is decided based on the clinical, microbiological and radiological criteria recommended by the American Thoracic Society/Infectious Disease Society of America guidelines. These include confirmatory microbiological findings of the presence of the same NTM species in culture of either one bronchoalveolar lavage or two sputum samples, or respiratory tissue demonstrating granulomatous histopathology.4
Pulmonary NTM is difficult to diagnose because of several factors, which include:
- low pathogenicity and indolent course
- environmental ubiquity, especially in water sources, often disregarded as a contaminant
- lack of physician awareness leading to it not being considered in the differential diagnosis, thus, ignoring features that may fulfil the diagnostic criteria.
Treatment
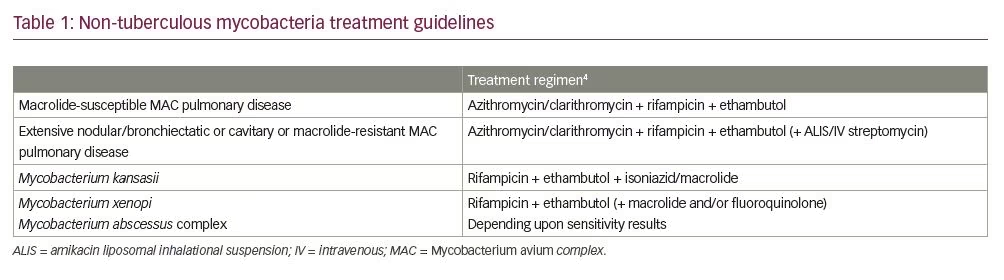
The initiation of treatment with antimicrobials depends on the pathogenicity and virulence of the NTM species detected, the clinical status of the patient, the risk-benefit assessment, and the pros and cons of therapy. In addition to the high costs, patients find it difficult to comply and adhere to the therapeutic regimen because of its long duration and numerous side effects.16 The recommended treatment regimens are outlined in Table 1.
Socioeconomic burden of non-tuberculous mycobacteria
While the morbidity and mortality of pulmonary NTM is significant in some cases, its socioeconomic impact is noteworthy. Patients with NTM have more comorbidities than those without NTM, as evidenced in a systematic review.18 It was further seen that patients with pulmonary NTM experienced worse health-related quality of life compared with those without NTM.19,20 These patients were three times more likely to be hospitalized and absent from their work compared with those without NTM infections. In addition, the mortality rate in patients with NTM is increased four-fold.21
Non-tuberculous mycobacteria or tuberculosis: the overlap and a clinical dilemma
It is undoubtedly true that, while the public health implications of TB are the major focus of TB control worldwide, the overlap between TB and NTM has some potential implications and ramifications. Both NTM and M. tuberculosis belong to the group of mycobacteria that have similar clinical and radiological presentations and pathologic processes that lead to tissue granuloma formation and caseating necrosis. With the lack of easy and quick availability of culture data, DNA probes, PCR and high-performance liquid chromatography testing, coupled with limited use of GeneXpert testing in Bangladesh, the distinction between TB and NTM at a clinical and patient level, and confirmation of the diagnosis, becomes difficult. This may result in double jeopardy of misdiagnosis of mycobacterial disease, both TB and NTM. This, in turn, has wider public health, clinical, environmental and financial implications for both the patient and the population.
At present, to the best of our knowledge, there is a lack of awareness among Bangladeshi physicians regarding NTM. A literature search on PubMed with the MeSH terms ‘non-tuberculous mycobacteria’ and ‘Bangladesh’ yielded only a single publication. Like other countries, it is not a requirement in Bangladesh to report NTM infections to the public health authorities. The first report on the presence of NTM in Bangladesh was published in 2017 when 74 (9.4%) NTM-positive samples were detected by PCR in 782 clinical specimens from patients with TB in a tertiary hospital in Dhaka. However, this study did not ascertain the incidence or prevalence of clinical infections.22 A case report published in 2017 described M. fortuitum isolated from a cutaneous abscess in a 45-year-old female patient with diabetes, later cured successfully with a combined regimen of amikacin, ethambutol and clarithromycin for 6 months’ duration.23 A study from 2015 to 2019 demonstrated the presence of NTM in breast lesions from nine patients, identified with the help of PCR.24 Although these publications confirm the presence of NTM in Bangladesh, they do not provide any robust data regarding the prevalence and clinical burden of NTM, and the geographical distribution of the various species in the country.
Non-tuberculous mycobacteria in South-east Asia and the Indian subcontinent
Compared to Pakistan and Bangladesh, where there have been few publications on NTM, numerous studies have been published from India.25–31 In northern India, pulmonary NTM is predominantly caused by M. intracellulare and MAC, followed by M. abscessus; whereas extrapulmonary disease is mostly caused by M. abscessus.26 However, in a study conducted by Maurya et al., M. fortuitum was found to be the most common organism isolated from extrapulmonary samples in northern India, followed by M. intracellulare, and M. abscessus.27 Umrao et al. found 29% prevalence of NTM among 906 pulmonary and extrapulmonary clinical specimens from northern India, which was predominated by M. abscessus, followed by M. fortuitum, M. intracellulare and M. chelonae.28 In the south Indian state of Tamil Nadu, Gomathy et al. found M. kansasii as the most abundant isolate among patients with pulmonary NTM, followed by M. intracellulare and M. abscessus.29 A retrospective analysis of clinical specimens in Chennai established M. chelonae as the most abundant NTM species, followed by M. fortuitum.30 Another retrospective study in India, conducted on 877 patients with suspected TB, observed an NTM prevalence of 3.8%, which included 19 pulmonary and 15 extrapulmonary cases of NTM.31
A cross-sectional study performed in a tertiary hospital in Pakistan found 104 (0.4%) NTM-positive samples from 25,955 clinical specimens. The bulk of the isolates were rapidly growing mycobacteria, with the most common organisms being M. fortuitum, followed by MAC and M. mucogenicum.32 In a study conducted to evaluate the prevalence of mycobacterial disease, an NTM disease prevalence of 2% was observed among 1,060 patients with HIV in Thailand and Vietnam.33
Studies have demonstrated that the distribution of NTM species varies with geographical location.6,12 The prevalence data from the neighbouring countries thus signal the possibility of a similar or higher prevalence in Bangladesh, and highlights the need for increased awareness and prevalence studies in this country.
Why should awareness of non-tuberculous mycobacteria be emphasized in Bangladesh?
With the high prevalence of TB, it is fiscally prudent, in terms of public health, that prevention of communicable diseases takes precedence; however, emerging pathogens like NTM, albeit clinically relevant to patient care, are often overlooked. The changing demographics of Bangladesh, and its unique ecological background, dictate that we remain aware of this problem and its potential direct and indirect impact on the management of mycobacterial disease.
Environmental public health concern
Bangladesh is a riverine country, lying in the Ganges delta system, which is one of the largest deltas in the world, with a river network spreading across the delta from India, Nepal, Bhutan and China into the Bay of Bengal. Bangladesh has three major river systems including 57 transboundary rivers.34 The coastal zone adjoining the Bay of Bengal is inhabited by approximately 25 million residents.35 As NTM are known worldwide to be prevalent in this ecosystem, with abundant rivers and estuaries, the population of Bangladesh could be at a high risk of being affected by NTM; thereby, potentially making it an important environmental public health concern for the country.
Overestimation of tuberculosis in Bangladesh? An intriguing hypothesis
It can be hypothesized that the high prevalence of TB in Bangladesh, if based on clinical history alone, could be attributed to its misdiagnosis as both NTM and TB stain positive on Ziehl–Neelsen stain. The Bangladesh National TB Program dictates the commencement of anti-TB treatment following acid-fast bacillus (AFB)-positive smears without confirmation with culture. This is to avoid treatment delay and reduce transmission of TB among the population.3 Although TB treatment success rates in Bangladesh have been estimated to be 94%, it should be noted that this is based on the rates of completion of treatment and not necessarily culture conversion. As both M. tuberculosis and NTM treatment involve similar drugs, treating patients with NTM who are misdiagnosed as having M. tuberculosis with only an anti-tubercular regimen could be of multi-faceted impact, both at the level of TB control and public health measures, contributing to the development of resistance against these drugs. One can hypothesize that inadequate detection of NTM can be one of the factors contributing to overestimation of TB as currently diagnosed.
Conclusion
NTM is an emerging worldwide problem that requires attention, as it can negatively impact the lives of the affected, both physically and financially. Physicians must consider NTM as a differential of TB while treating a patient. It is imperative that the accurate diagnosis of TB with more robust and standardized methodology with culture and GeneXpert is adopted, as it is crucial to the accurate diagnosis, treatment and estimation of the true burden of TB in Bangladesh. While treatment for TB is urgent and based on the pre-test likelihood and regional prevalence of the disease, it may not be prudent to label all persons with a positive AFB smear as having TB without confirmatory diagnosis on culture and GeneXpert tests, as this may underestimate the prevalence of NTM. This is especially applicable in countries like Bangladesh, where resources have to be distributed effectively. Furthermore, laboratories across Bangladesh must be equipped with diagnostic facilities to identify and differentiate NTM species to select the most appropriate and cost-effective treatment regimens when indicated. The prevalence and clinical, environmental and public health ramifications of NTM in Bangladesh must be recognized and studied, as they may impact the management of mycobacterial disease at the patient and public health levels, and aid in formulating health policy in the future.







