Aspirin-exacerbated respiratory disease (AERD) is a clinical triad of asthma, nasal polyposis and sensitivity to aspirin and other non-steroidal anti-inflammatory drugs (NSAIDs). These patients have severe sinopulmonary inflammation, often refractory to standard treatments.1 However, significant advances in the management of both asthma and nasal polyposis allow for new treatment options and management algorithms. This article aims to review the most recent clinical updates of AERD prevalence, diagnosis and management. Recent clinical studies with relevance to patients with AERD are reviewed.
Prevalence
For the estimated 2 million patients with AERD living in the United States, AERD represents a significant healthcare burden, costing over US$4.5 billion, annually.2 It is thought that 8–26% of patients with nasal polyposis and 7.2% of patients with asthma have AERD.2,3 However, the true prevalence of AERD is unknown, as aspirin challenge is underused.4 A history of sensitivity to aspirin or NSAIDs is suggestive of AERD, but a lack of such a reaction does not rule it out. It has been shown that 30–40% of patients with nasal polyps who feel they are tolerant to aspirin actually have a positive aspirin challenge.2
Pathophysiology
The sinopulmonary symptoms seen in AERD are due to recalcitrant type-2 inflammation. The inflammatory profile stems from baseline dysregulated arachidonic acid metabolism, mast cell activation and blood and airway eosinophilia.5 Dysfunctional metabolism of arachidonic acid has been found to be the key mediator in AERD pathogenesis.6 At baseline, patients with AERD have decreased cyclooxygenase-2 (COX-2) and prostaglandin E2, resulting in decreased prostaglandins and increased pro-inflammatory pro-leukotrienes. Therefore, cyclooxygenase-1 (COX-1) inhibitors shunt arachidonic metabolism further towards the pro-leukotriene pathway, causing a characteristic acute increase in inflammatory symptoms, often presenting as respiratory, and occasionally, systemic reactions. The downstream product, urinary leukotriene E4 (uLTE4), is elevated in patients with AERD, and has been shown to elevate further during NSAID-induced reactions, such as aspirin desensitization.6 Consequently, uLTE4 has been the focus of significant research as a potential biomarker of AERD diagnosis and severity, although it remains undetermined.7 Importantly, patients with AERD tolerate COX-2 inhibitors.8
Diagnosis
AERD is usually diagnosed in the third or fourth decade of life.9 The natural history involves chronic rhinosinusitis that evolves into manifestations of lower airway inflammation, and subsequently, NSAID hypersensitivity. Upper airway symptoms include nasal congestion, facial pressure/pain, rhinorrhoea, loss of smell and sneezing, while lower airway symptoms include laryngospasm, coughing, wheezing and shortness of breath.1 As a systemic disease, patients may experience gastrointestinal manifestations, primarily abdominal pain, and cutaneous symptoms, such as flushing and urticaria.1 These symptoms can develop independently, and are characteristically exacerbated by aspirin and other NSAIDs. The presentation with these symptoms alone is often insufficient for diagnosis, and aspirin challenge may be necessary for confirmation. Interestingly, upper airway symptoms, including rhinitis, often precede the lower airway symptoms of asthma by 1–5 years.10 The chronology of symptoms seems to mimic an ‘allergic march’, seen in atopic disease, although AERD does not represent a true allergy. Although patients may present with anaphylaxis-like attacks, symptoms of AERD are not immunoglobulin E (IgE) mediated.11 However, environmental allergies and AERD may co-exist.12
The diagnosis of AERD may be difficult, as up to 15% of patients with AERD are unable to identify if they are sensitive to NSAIDs.9 The reasons for this are multifactorial, and include recommended NSAID avoidance following the development of asthma and nasal polyps. Occasionally, patients may even tolerate low-dose aspirin therapy.13
The aspirin provocation challenge, performed in a monitored setting, is the gold standard for the diagnosis of AERD. A challenge is considered positive in the event of naso-ocular and/or lower respiratory reactions, and if forced expiratory volume in 1 second (FEV1) decreases by >15%. The aspirin challenge is safe when preceded by a pre-treatment strategy, including oral corticosteroids and leukotriene-modifying drugs, but should not be offered if the baseline FEV1 is <70%, or if there is a history of a severe reaction or anaphylaxis to aspirin or other NSAIDs. While it is an integral part of AERD diagnosis, unfortunately the aspirin challenge is underused.4 In a survey of physicians by the American Academy of Allergy, Asthma and Immunology (AAAAI), aspirin challenge was not offered by 37.5% of respondents, and 28.2% did not refer patients to a provider who would perform the challenge.14 Consequently, there exists an undiagnosed and therefore undertreated population with AERD.
Beyond sensitivity to aspirin, other clues in a patient’s history may suggest AERD. Smoking cessation has been found to be a risk factor for AERD.15 Of 114 patients with AERD, Hayashi et al. found that, with the onset of symptoms, 20% had recently quit smoking and were 4.63 times more likely to have recently quit compared with patients with aspirin-tolerant asthma.15 The underlying mechanism is likely the pro-inflammatory environment caused by smoking, which increases COX-2 expression. In addition, up to 75% of patients with AERD also display sensitivity to alcohol, with flushing, wheezing and urticaria.16 The mechanism is largely unknown, but may be related to polyphenols present in alcohol, which are known inhibitors of COX-1.17 However, this phenomenon is observed less frequently in patients with aspirin-tolerant asthma, allergic rhinitis and even in healthy controls as compared to AERD. Importantly, patients often tolerate alcohol after aspirin desensitization or dupilumab therapy.18,19 This unique aspect of therapy may be a motivating factor for some patients to undergo these treatments.
Treatment
Avoidance
As AERD is exacerbated by aspirin or NSAID ingestion, it seems appropriate that salicylate avoidance would appropriately control symptoms. However, baseline symptoms of AERD tend to be progressive, even with strict NSAID avoidance, as COX-1 inhibition is not necessary to either initiate or sustain the disease. While additional study is required, exposure to dietary non-acetylated salicylates may contribute to this baseline inflammation.12 High-salicylate beverages include alcohol, carbonated drinks and coffee; high-salicylate foods include starches, leafy greens and most fruits. In 2015, Sommer et al. performed a prospective, cross-over, pilot study in 10 patients randomized to 6 weeks of either a regular diet or a low-salicylate diet. Results showed improved nasal symptoms and endoscopy scores in the patients on a low-salicylate diet.20 A follow-up prospective, cross-over study was recently performed, which randomized seven patients to either a high- or low-salicylate diet for 1 week. While there was no statistical difference in the urinary salicylate and leukotriene levels between the two diets, patients on the low-salicylate diet had improved sino-nasal outcomes test (SNOT-22) scores.21 Given the fact that low-salicylate diets are highly restrictive, further research is needed to support these findings.22 In addition, dietary omega-3 and omega-6 fatty-acid intake may play a role in disease control by targeting arachidonic acid dysregulation. A prospective, non-blinded study of 10 patients with AERD found a diet reduced in omega-6 fatty-acid consumption with increased omega-3 intake led to reductions in both uLTE4 and SNOT-22 scores, compared with baseline.23
Topical therapy
As an inflammatory process of the upper and lower airways, topical corticosteroid treatment is standard therapy for both the asthma and nasal polyps seen in AERD. While the use of multiple inhalers (including short- and long-acting b agonists) may be sufficient to manage lower airway disease, patients with asthma and comorbid AERD are significantly more likely to be oral-corticosteroid dependent than patients with chronic rhinosinusitis with nasal polyposis (CRSwNP) and asthma.24 Similarly, topical corticosteroid sprays in the nasal cavity are less successful in controlling upper airway symptoms in patients with asthma and AERD than in patients with CRSwNP;25 and unoperated sinuses prevent deep penetration of topical steroid sprays. Furthermore, patients with AERD often have significant nasal polyp burden, resulting in poor corticosteroid distribution. High-volume rinses with off-label corticosteroids, such as budesonide or mometasone, may improve medication delivery. The recent development of novel steroid delivery devices, such as Xhance® (OptiNose US, Yardley, PA, USA), has shown promise in patients with nasal polyposis.26 As AERD is often recalcitrant, these delivery devices may be an alternative after exhausting other medical options.
Oral therapies
A hallmark of AERD is cysteinyl leukotriene overproduction, which is elevated further during acute inflammatory events brought on by aspirin or NSAIDs.27 Pro-inflammatory leukotrienes underpin the pathogenesis of AERD; therefore, leukotriene-modifying drugs are a viable option. Montelukast and zafirlukast work as cysteinyl leukotriene receptor 1 (CysLT1) antagonists and are an integral component of aspirin desensitization safety.28 While they are often included in the medical regimen of patients with AERD, their benefits in controlling both upper and lower airway symptoms are less clear. Similarly, zileuton acts as a partial inhibitor of 5-lipoxygenase, halting downstream leukotriene formation.29,30 A recent review of 45 patients with AERD found that those taking zileuton had slightly reduced rates of surgical intervention (though not statistically significant) compared with those not taking the medication; however, no benefit was seen in other rhinologic quality-of-life outcomes.29 The side effects of these drugs must also be considered. Montelukast carries a risk of mental health side effects, including completed suicide.31 Zileuton carries a risk of self-limited hepatotoxicity, which requires liver function monitoring.32
As with other forms of asthma and chronic rhinosinusitis, judicious use of oral steroid therapies provides short-term benefits in patients with AERD. Oral steroids are often best employed in the perioperative period to reduce polyp regrowth after functional endoscopic sinus surgery.22
Aspirin desensitization
Aspirin desensitization therapy was discovered unintentionally at the Scripps Clinic (San Diego, CA, USA) in the late 1970s during aspirin challenge clinical trials.33 Aspirin desensitization is not directly analogous to other inhalant/medication allergen desensitization, as the underlying mechanism of aspirin desensitization remains unknown. Despite this, there have been several double-blind, placebo-controlled studies demonstrating the benefits of aspirin desensitization.34 Principally, long-term, high-dose aspirin therapy affords significant improvement in upper airway symptoms, decreased polyp recurrence, fewer revision surgeries and improved quality-of-life metrics as compared to placebo.34–36 However, through all these trials, it should be noted that desensitization is difficult to blind, as symptoms will characteristically develop with aspirin ingestion.
Historically, patients were given incremental doses of aspirin until 650 mg twice daily was tolerated. However, multiple trials have demonstrated a benefit at lower doses. In a trial of 40 patients, as low as 300 mg per day was found to be effective.36 Although there was no comparison group, the investigators found favourable outcomes, including fewer episodes of sinusitis and revision surgeries, and improved nasal congestion and sense of smell.36 Furthermore, a study performed in 2013 compared just 100 mg/day aspirin against placebo.35 With 70 initial participants, 31 individuals were evaluated at 36 months. The authors reported that the aspirin group had reduced nasal polyp relapse. It should be noted, however, that a major limitation of this study was the high dropout rate and patients with AERD were selected based on history and in vitro testing. A recent work-group report recommends the maintenance dose of aspirin start at 650 mg twice daily for 1–6 months, with step down thereafter to 325 mg once or twice daily for patients who are doing well. If symptoms worsen following the step down, the dose should be increased back to 650 mg twice daily.37
Aspirin challenges and desensitization are typically performed in an outpatient setting, although prior to the adoption of pre-medication protocols this was frequently completed in the intensive care unit. Aspirin challenges are performed to confirm underlying AERD, whereas aspirin desensitization is indicated for patients who need long-term, high-dose aspirin therapy. The protocol used for both procedures is identical, and both aspirin challenges and desensitization involve invoking symptoms of AERD. Characteristic upper and lower airway symptoms occur within 40–60 minutes. To minimize these reactions, most aspirin challenges move immediately to desensitization. Ocular and gastrointestinal symptoms may also develop.38
Most protocols are complete by 24–48 hours of therapy, and several different protocols exist.39,40 Patients should be monitored for at least 3 hours following an aspirin-induced reaction during challenges and desensitization until symptom resolution. The protocol is stopped thereafter in a challenge, whereas in a desensitization, the provoking dose is re-administered and the protocol continued through to 325 mg of aspirin. It is important to note that not all protocols use oral aspirin for desensitization. Many European countries use ketorolac or other NSAIDs, as well as intranasal administration. Desensitization continues for at least 6 months, and if effective, indefinitely.39 If side effects arise, aspirin therapy should be discontinued at any point. In addition, it should be noted that the desensitization itself is not beneficial, but rather the daily maintenance dose of aspirin following desensitization is what produces the therapeutic effect.35
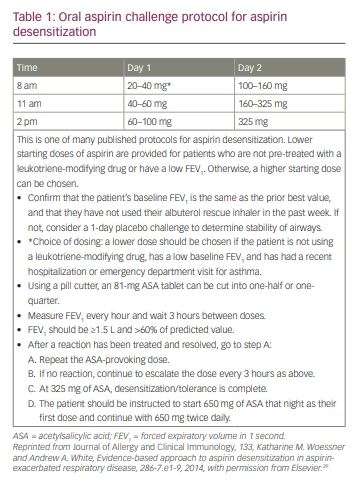
Prior to desensitization, patients are typically pre-medicated with leukotriene inhibitors, with oral-corticosteroids being reserved for patients with tenuous asthma control. A full ‘crash-cart’ or airway box is required, stocked with appropriate medications including epinephrine and antihistamines. Patients undergoing desensitization may continue their biologics and inhaled corticosteroids. Incentive spirometry is used to monitor FEV1 closely.41 A widely used protocol from Scripps Clinic starts the first day with 20–40 mg of aspirin, doubling the dose every 3 hours for 6 hours.39 The following day, the dose starts at 100–160 mg of aspirin and increases every 3 hours until 325 mg is tolerated. That night, the patient is desensitized and takes 650 mg of aspirin. FEV1 should be checked every hour and remain >1.5 L or >60% of the predicted value. With this protocol, patients are desensitized over 2 days during office hours. This protocol is summarized in Table 1.39 It should be noted that there are recent published trials demonstrating success in just 1 day of the oral aspirin challenge.42 Furthermore, intranasal ketorolac challenge and desensitization followed by rapid oral aspirin challenge is also safe and less time-consuming than the standard oral aspirin desensitization protocol.43
While aspirin desensitization is generally safe, there are contraindications. Patients who are pregnant, have unstable asthma, gastric ulcers, eosinophilic oesophagitis or are taking other anticoagulants are not candidates for chronic aspirin therapy. In addition, patients under the age of 14 years should not take aspirin due to the risk of Reye’s syndrome.37
Surgical management
As a difficult-to-treat variant of chronic rhinosinusitis with nasal polyposis, surgical management of AERD with endoscopic sinus surgery is routine after the failure of appropriate medical therapy. In patients with AERD, endoscopic sinus surgery generally includes the opening of all sinuses. Despite this, the failure rate is high, and many undergo revision, with rates ranging from 38–89%.44,45 The literature generally agrees that ‘full-house’ endoscopic sinus surgery, or the opening of all the paranasal sinuses, is indicated for patients with AERD, though the extent of frontal sinus surgery remains controversial. Some advocate for an upfront Lothrop or Draf III procedure, whereby the bilateral frontal sinuses are made into a common cavity by removing portions of the intersinus septum and middle turbinate attachments.46 In a prospective study of 31 patients with AERD who underwent a Lothrop procedure, in addition to standard endoscopic sinus surgery, a failure rate of 22.5% was reported, whereby patients required revision surgery.47 While upfront, maximum-extent, sinus surgery with a Lothrop procedure is an option, the failure rate remains high, highlighting the need for adjunctive therapy. Therefore, the best outcomes occur with strong multidisciplinary care between the surgeon and allergy/immunology colleagues.
Given the well-studied benefits of aspirin desensitization, this therapy is commonly started 2 weeks after surgery to minimize the bleeding risk. The complementary nature of surgery with long-term, high-dose aspirin therapy was evidenced by Jerschow et al. in 2019.48 A total of 28 patients underwent aspirin challenge before endoscopic sinus surgery to confirm a diagnosis of AERD. Next, 2–3 weeks after surgery, these patients underwent aspirin challenge followed by aspirin desensitization. Aspirin challenge following endoscopic sinus surgery resulted in less-severe reactions in all patients, and 43% of patients had no detectable reaction to aspirin. This suggests that decreasing the polyp load decreases the systemic reaction to aspirin. Furthermore, the reduced severity of reaction to aspirin was linked to certain biomarkers, as these patients had increased lipoxin A4, and decreased uLTE4 and prostaglandin D2. Overall, their prospective observational trial demonstrated that aspirin challenge was safer after endoscopic sinus surgery.48
Medical management: biologics
Despite appropriate medical and surgical management, many patients with AERD remain symptomatic. Some may also not derive benefit from, nor tolerate chronic aspirin therapy. Biologic therapy targeting Th2 inflammatory pathways has recently become a therapeutic alternative. Dupilumab, omalizumab and mepolizumab are options for use in moderate-to-severe asthma, and have been studied in patients with AERD.49
Dupilumab, approved by the US Food and Drug Administration (FDA) in June 2019 for nasal polyps, is an antagonist of the interleukin-4 receptor (IL-4R) α subunit, modulating both the IL-4 and IL-13 pathways.50 Prior studies have shown the effectiveness of dupilumab in treating patients with CRSwNP,51 with parallel reduction in local Th2 pro-inflammatory biomarkers on nasal secretion analysis.52 Furthermore, in a nested analysis of the phase II dupilumab trial, patients with CRSwNP and underlying AERD (19 patients of 60) demonstrated greater improvements in nasal polyp and SNOT-22 scores compared with the rest of the cohort.53 In 2020, Mustafa et al. followed 10 patients with AERD treated with placebo for 1 month, followed by dupilumab as add-on therapy for 6 months.19 In addition to improved SNOT-22 and Lund–MacKay computed tomography scores, most patients also had improved tolerance to alcohol, a result which was reproduced in a separate case series.54
While omalizumab (anti-IgE) has been approved by the FDA for asthma and idiopathic urticaria since 2003, in December 2020, it joined dupilumab as the only other FDA-approved biologic for nasal polyps.55,56 Omalizumab is effective in reducing allergic inflammation by binding circulating IgE. It has been found to be effective in relieving nasal symptoms of patients with AERD, but currently, there is no evidence that it prevents polyp recurrence after surgery.57 In a case series of 29 patients, omalizumab reduced the number of oral steroid courses along with short-acting
b agonist use.58 Following this, a randomized, placebo-controlled, double-blind, crossover-trial of 16 patients with AERD, by Hayashi et al. in 2020, demonstrated decreased uLTE4 and reduced upper and lower respiratory tract symptoms after 3 months of omalizumab during oral aspirin challenge.59 However, in two phase III studies of omalizumab in patients with nasal polyps, 40 of 265 patients had underlying AERD, and demonstrated similar mean improvements in nasal polyp score at week 24 compared to patients without AERD.60
Mepolizumab binds to and inhibits IL-5, preventing the binding with and activation of eosinophils. While a small trial of 20 patients with nasal polyps showed a reduction in polyp size in 12 patients, it remains unclear if mepolizumab provides any specific additional benefit in AERD.49,61 Mepolizumab was specifically evaluated in a small retrospective study of 14 patients with AERD, and there was a consistent trend towards decreased SNOT-22 scores, improved sense of smell and improved nasal congestion scores, compared with baseline.62 A subgroup analysis of the recent phase III study of mepolizumab in patients with nasal polyps also suggested higher efficacy compared with placebo in patients with AERD, based on greater improvement in visual analogue scale score in this population.63
With promising early data, future studies of biologics in the treatment of AERD will bring more evidence to the decision-making process. While there are some data supporting the efficacy of omalizumab and mepolizumab, dupilumab currently carries the most evidence of success in treating patients with AERD.19,53,51 Future head-to-head trials are eagerly awaited. In addition, there are several other biologics in the pipeline, directed against various signalling molecules in the type 2 inflammatory cascade, such as cytokine thymic stromal lymphopoietin (TSLP), which is a significant contributor to the pathophysiology of AERD.64 However, access and cost remain significant barriers to their widescale use. Biologics cost $30,000–40,000/year, with variable cost to payors and patients.25 In addition, studies have yet to examine the specific role of biologics after endoscopic sinus surgery; surgery was considered an outcome measure in the aforementioned trials.51,52,61 Certainly, with the known benefit of aspirin desensitization after endoscopic sinus surgery, the additional role for biologics in this setting remains unclear.
Management strategy
Although AERD has a reputation as a recalcitrant disease, presentation and response to treatment is often along a spectrum. With a growing assortment of treatment options, it is paramount to individualize therapy alongside a stepwise algorithm. Patients with AERD should begin with appropriate medical management, including saline irrigations, topical nasal corticosteroids, anti-leukotrienes and the occasional course of oral steroids.25 For those that fail, comprehensive sinus surgery is indicated. For those that relapse after a first surgery, a revision with a Lothrop procedure is indicated, unless the first surgery was felt to be inadequate.47 Either with early polyp recurrence or, if indicated, following the second endoscopic sinus surgery, adjunctive medical therapies, such as aspirin desensitization, are essential. Patients with polyp recurrence after surgery may be candidates for revision surgery, and removal of these polyps facilitates safe aspirin desensitization and prevents relapse. If aspirin desensitization fails, or is otherwise unable to be tolerated, biologics are an appropriate alternative.48,51







